 There’s a lot of information about the importance of friendly bacteria to the gastrointestinal tract. Intestinal microflora also called friendly flora or probiotics, play a role in regulating the immune system and keeping the colon healthy. However, most of the bacteria in your intestines should be in your colon or large intestines, not your small intestines.
There’s a lot of information about the importance of friendly bacteria to the gastrointestinal tract. Intestinal microflora also called friendly flora or probiotics, play a role in regulating the immune system and keeping the colon healthy. However, most of the bacteria in your intestines should be in your colon or large intestines, not your small intestines.
When abnormally large numbers of bacteria (even friendly bacteria) start growing in the small intestines, they actually cause problems with your health. Small Intestinal Bacterial Overgrowth (SIBO) is a condition where abnormally large numbers of bacteria are present in the small intestines.
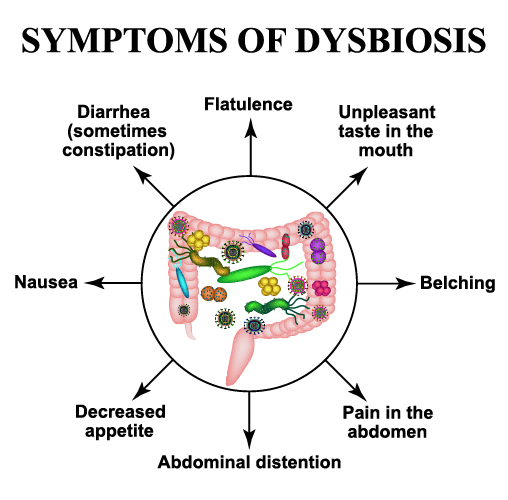
These bacteria feed off of sugars and starches in the diet (both refined sugars and natural sugars) and produce methane and hydrogen gas. They also inhibit the enzymes in the small intestines that break down starches into simple for absorption. This can result in abdominal bloating, belching, and/or flatulence (intestinal gas), especially when you eat grains and other complex carbohydrates. The gases produced by these bacteria can also cause abdominal pain, intestinal cramping, and IBS with constipation and/or diarrhea. Gas pressure in the small intestines can push upwards against the stomach, contributing to the development of a hiatal hernia and causing heartburn, acid reflux, GERD, and nausea.
SIBO increases a hormone called zonulin causing an increase in small intestinal permeability (aka leaky gut syndrome), which results in the intestines absorbing large molecules they shouldn’t. The bacteria also like to gobble up essential nutrients like fats, iron, and vitamin B-12. The nutrient deficiencies from SIBO along with the absorption of large protein molecules can cause problems with the immune system and can contribute to allergies, asthma and autoimmune disorders, and a general decline in health.
SIBO has wide-ranging implications and may be a cause or a major factor in all of the following diseases: acne rosacea, acne vulgaris, acromegaly, anemia, autism, celiac disease, CLL (chronic lymphocytic leukemia), cystic fibrosis, chronic fatigue syndrome, diabetes, diverticulitis, erosive esophagitis, fibromyalgia, gastroparesis, GERD (gastroesophageal reflux disease), H. pylori infection, hypochlorhydria (low stomach acid), hypothyroid/Hashimoto's thyroiditis, IBD (inflammatory bowel disease) such as Crohn’s and ulcerative colitis, IBS (irritable bowel syndrome), interstitial cystitis, lactose intolerance, liver cirrhosis, Lyme disease, malabsorption syndrome, muscular dystrophy (myotonic type 1), NASH/ NAFLD (non-alcoholic steatohepatitis/non-alcoholic fatty liver disease), obesity, pancreatitis, parasites, Parkinson's, prostatitis (chronic), rheumatoid arthritis and scleroderma (systemic sclerosis). Please note, this does NOT mean that SIBO causes all these diseases, it just means that it may be a contributing factor or may accompany these conditions.
Other clues that SIBO may be a problem include having better bowel movements after taking antibiotics and having bowel problems get worse when taking probiotics or fiber. If bowel problems began after using opiates for pain, this is another clue that SIBO may be a factor.
Do You Have SIBO?
 Experts in SIBO have estimated that about 35-50% of the general public has this problem. Unfortunately, it is not widely understood and hence, is not properly diagnosed. Many people who have SIBO think they have a Candida or yeast infection. However, while yeast overgrowth can occur with or without SIBO, Candida is often overdiagnosed and SIBO is underdiagnosed. Fortunately, the protocols are similar, but the treatment is different enough that people with SIBO may not respond well to a Candida or yeast program and be discouraged by the lack of results.
Experts in SIBO have estimated that about 35-50% of the general public has this problem. Unfortunately, it is not widely understood and hence, is not properly diagnosed. Many people who have SIBO think they have a Candida or yeast infection. However, while yeast overgrowth can occur with or without SIBO, Candida is often overdiagnosed and SIBO is underdiagnosed. Fortunately, the protocols are similar, but the treatment is different enough that people with SIBO may not respond well to a Candida or yeast program and be discouraged by the lack of results.
A medical diagnosis of SIBO is difficult because it is hard to get a culture from the small intestines. There are tests involving collecting breath samples from patients that drink either glucose or lactulose. The lactulose test is the most accurate. These tests must be ordered by a physician.
However, you can also assess this condition fairly accurately by symptoms. If you have an auto-immune disorder, pain in multiple joints, chronic allergies, chronic skin conditions, chronic fatigue or depression or general malaise (just don’t feel good) you may have leaky gut. When you have symptoms of leaky gut coupled with chronic diarrhea or constipation, regular abdominal pain, IBS, bloating or belching after meals, GERD, and/or regular indigestion, you may have SIBO.
What Causes SIBO?
 There are several major factors that contribute to the development of SIBO. The first is a lack of hydrochloric acid (HCl) in the stomach. HCl helps the body digest proteins, but it also helps to kill bacteria in the food we eat and prevent them from colonizing the small intestines.
There are several major factors that contribute to the development of SIBO. The first is a lack of hydrochloric acid (HCl) in the stomach. HCl helps the body digest proteins, but it also helps to kill bacteria in the food we eat and prevent them from colonizing the small intestines.
A second factor is a lack of intestinal motility. In between meals migrating motor complexes (MMCs) sweep down the intestines, helping to flush bacteria. These movements of the small intestine are what are responsible for what we call hunger pains, the “rumblings” we feel in our gut when we haven’t eaten in a while. These MMCs may be damaged by surgery, intestinal scarring, various diseases, intestinal infections, and by certain drugs. Medications that can inhibit these intestinal movements include antibiotics, proton pump inhibitors, antacids, and opiates (pain killers) like morphine.
Stress can be a factor in both low hydrochloric acid and the lack of intestinal motility as the sympathetic nervous system (responsible for the fight or flight response) inhibits both digestive secretion and intestinal motility. When we are relaxed, the parasympathetic nervous system is more active and digestion and intestinal motility are enhanced. Unfortunately, many people in our society are eating on the run and do not take time to relax, chew their food thoroughly, and enjoy their meals.
A final factor in SIBO is a malfunctioning ileocecal valve. This valve is between the small and large intestines and is designed to prevent backflow (that is, to keep material in the large intestine from migrating back into the small intestine. When this valve is not shutting properly, intestinal bacteria migrate from the colon into the small intestine causing gas, bloating and general weakness and malaise.
Natural Therapy for SIBO
Here are seven things you can do to overcome SIBO. Many of these things are also done for leaky gut.
Step One: Remove food and chemical irritants
Dietary adjustments are essential to overcoming both SIBO and leaky gut. It is absolutely essential to eliminate all refined sugars from the diet and most starchy foods. At the least one should eliminate all grains containing gluten (wheat, rye, barley), but eliminating all grains may be required.
Dairy may also be problematic because the bacteria love to feast on the sugar in dairy, lactose. . Goat milk products, and cultured dairy foods can be beneficial for some people, yet other people may have to eliminate all dairy foods. Fermented foods are generally helpful for SIBO. These are discussed under Step Six: Restore beneficial bacteria.
There are three dietary programs that may be helpful, depending on the severity of the problem. These are the Specific Carbohydrate Diet (SCD), the Gut and Psychology Syndrome (GAPS) diet, and the Paleo diet. Resources on all three of these diets can be found at the end of this article.
Step Two: Stimulate the production of and/or supplement stomach acid and enzymes
 There are two ways to increase stomach acid and enzymes. One is to take supplements and the other is to take herbs and nutrients that stimulate their production. With SIBO it is normally necessary to do both.
There are two ways to increase stomach acid and enzymes. One is to take supplements and the other is to take herbs and nutrients that stimulate their production. With SIBO it is normally necessary to do both.
To determine how much Betaine HCl one needs you can do a hydrochloric acid challenge test. Note: do not perform this test if you have an active ulcer or a history of ulcers.
To do the test, take a 400-500 mg. capsule of betaine HCl with pepsin prior to a meal. If you notice no burning, you increase to two capsules the next meal. Proceed until you notice a mild burning sensation, then immediately reduce your dose to the number of capsules that preceded the burning or heat sensation. Most people find a comfortable dose between 400 and 1500 mg per meal (2-3 capsules).
If one or two capsules cause burning, you either don’t have low stomach acid or your reflux is so severe that you won’t be able to take HCL until you get it under control. Also, remember that the more protein you eat at a meal, the greater the need for HCl, so you can vary the dose with the size and content of your meals. Also, if you have severe digestive problems, you may also wish to take a complete food enzyme that has HCl and pancreatic enzymes.
Within 3-6 months most people feel a warmth in their stomach with the same dose they have been taking. When this happens it is time to decrease your dose and start weaning off of Betaine HCl.
 You can also use Herbal Bitters Formulas to stimulate digestive secretions. There are many versions of these digestive bitter tonics in the marketplace. Common ingredients in them include bitters herbs such as dandelion root, gentian, Turkey rhubarb, and burdock. They also contain aromatic herbs that stimulate digestion and ease gas and bloating, such as anise, ginger, peppermint, and cardamon. Orange peel and chamomile, both of which are bitter and aromatic are also common ingredients. Whatever ingredients the formula contains, it must taste bitter to work properly.
You can also use Herbal Bitters Formulas to stimulate digestive secretions. There are many versions of these digestive bitter tonics in the marketplace. Common ingredients in them include bitters herbs such as dandelion root, gentian, Turkey rhubarb, and burdock. They also contain aromatic herbs that stimulate digestion and ease gas and bloating, such as anise, ginger, peppermint, and cardamon. Orange peel and chamomile, both of which are bitter and aromatic are also common ingredients. Whatever ingredients the formula contains, it must taste bitter to work properly.
Bitters not only stimulate HCl secretion, they also stimulate pancreatic enzymes and bile from the gallbladder and tend to be mildly antibacterial as well. Bitters should be taken 15-20 minutes prior to meals with one to two large glasses of water. A small pinch of a natural salt can also be taken at the same time, as this also helps stimulate HCl production by providing chloride.
Bitters are contraindicated if you have digestive atrophy. So, if you have dry mucus membranes, as evidenced by a dry and withered (or shriveled) looking tongue, don’t take bitters as they dry the mucus membranes.
A lack of HCl may also be due to a lack of the following nutrients: chloride (low serum levels), zinc, and thiamine. These are the primary nutritional factors required for the synthesis of hydrochloric acid.
Step Three: Improve intestinal motility (if necessary)
With SIBO it is also important to make certain that there is good intestinal motility between meals to flush the intestines and clear out bacteria. One way to do this is to allow adequate time between meals. Depending on the efficiency of your digestion, you need three and five hours between meals. Ideally, you should wait until you get stomach rumblings indicating your digestive tract is clear before eating the next meal.
If motility is slow there are some supplements that may be helpful. All carminatives increase digestive motility, and many people find that a cup of ginger tea is most helpful. You can also try taking 100 mg of 5-HTP twice daily or MotilPro from Pure Encapsulations (two capsules twice daily). If improvement isn’t noted after two weeks, add 6 mg. of melatonin before bed and three capsules of Methyl Guard (Thorne) twice daily.
Step Four: Close the ileocecal valve (if necessary)
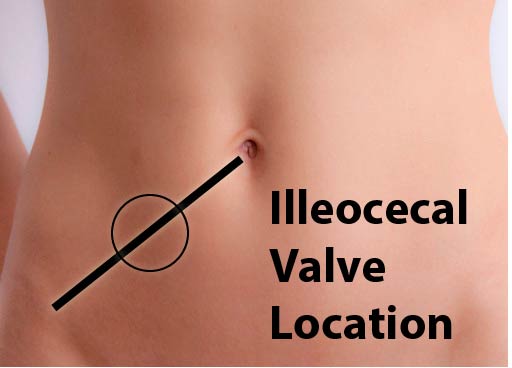 If there is severe gas and bloating, you probably need to work on the ileocecal valve. This is done by massaging the valve to reduce swelling and inflammation and get it to close properly. The ileocecal valve is located on the lower right side of the abdomen, midway between the belly button and the right hip bones as illustrated. Check the circled area shown in the picture to see if there is any swelling or tenderness in that area. If there is, massage the area a couple of times a day until the swelling and tenderness go away.
If there is severe gas and bloating, you probably need to work on the ileocecal valve. This is done by massaging the valve to reduce swelling and inflammation and get it to close properly. The ileocecal valve is located on the lower right side of the abdomen, midway between the belly button and the right hip bones as illustrated. Check the circled area shown in the picture to see if there is any swelling or tenderness in that area. If there is, massage the area a couple of times a day until the swelling and tenderness go away.
This is demonstrated in Steven’s article and videos on Correcting a Hiatal Hernia.
Step Five: Reduce bacterial overgrowth
If a person has signs of SIBO, they will need to take some supplements to reduce bacterial overgrowth in the small intestines. This can be done with pharmaceutical antibiotics or herbal antibacterial agents.
For starters, one can take an Herbal Bitters Formula with antibacterial herbs in it, instead of just plain digestive bitters. Ingredients to look for here include black walnut, goldenseal, andrographis, cat's claw, and Oregon grape.
Another great remedy is enteric-coated peppermint oil. Take one capsule with three meals each day for about 20 days. In clinical trials, this was shown to cause a 25-50% reduction in small intestinal bacteria. You can also make a type of coated peppermint oil by melting coconut oil at low heat, adding peppermint oil, then cooling it rapidly in the fridge. You can eat small amounts of this peppermint-flavored coconut oil several times daily. Another option is to take peppermint spirits, which is peppermint oil dissolved in alcohol.
Garlic is another possible antimicrobial agent, but if friendly Lacto bacteria are overpopulating the small intestines, it won’t work. It does kill gram-negative bacteria. The best way to take it is to chop up or crush fresh garlic, then mix it with a teaspoon of honey to make it easier to take. Encapsulated garlic products are generally ineffective.
Cinnamon kills both lactic acid bacteria and yeast. It is much more active than peppermint. Use it when you are sensitive to taking probiotics. Take two capsules three times daily with meals. I created a Cinnamon-Nopal Blood Sugar Formula for a major herb company that works well, too.
Goldenseal may also be helpful. It not only reduces intestinal bacteria, it also tones up digestive membranes and reduces irritation. It does lower blood sugar levels, however. Take two capsules three times daily with meals.
Note: It is not necessary to take ALL of the above remedies. That would be overkill. Pick one or two only, depending on your circumstances and what’s available to you.
Step Six: Restore beneficial bacteria
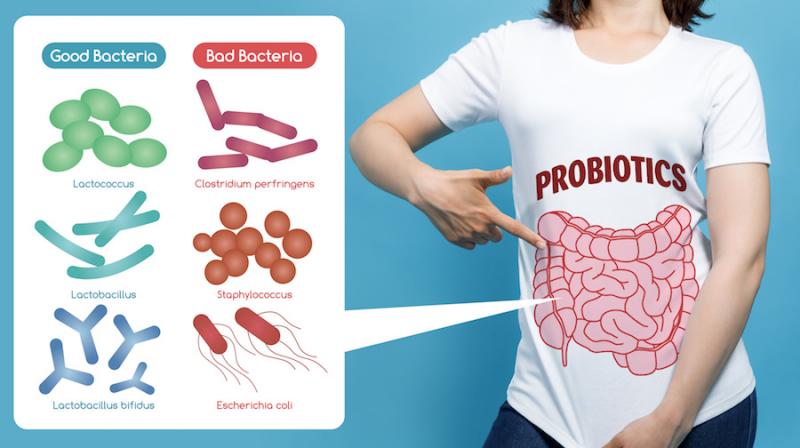 All traditional cultures used some kind of cultured foods. Vegetables were commonly cultured, but so were fruits and dairy foods. Studies have shown that it takes 10 billion encapsulated bacteria to obtain the same value to the intestines that just 100 million bacteria from food will do. Furthermore, people with SIBO often do not do well on probiotic supplements, especially if they contain prebiotics that feed the small intestinal bacteria as well as friendly flora.
All traditional cultures used some kind of cultured foods. Vegetables were commonly cultured, but so were fruits and dairy foods. Studies have shown that it takes 10 billion encapsulated bacteria to obtain the same value to the intestines that just 100 million bacteria from food will do. Furthermore, people with SIBO often do not do well on probiotic supplements, especially if they contain prebiotics that feed the small intestinal bacteria as well as friendly flora.
Cultured vegetables are very valuable in treating SIBO and leaky gut. You can make your own cultured vegetables or you can purchase them from a health food store or some supermarkets. Here are some brands of naturally fermented vegetables:
Making your own cultured vegetables is quite easy. Recipes for making cultured vegetables can be found in the materials from our Leaky Gut and SIBO webinar, online or from the book Nourishing Traditions by Sally Fallon.
Step Seven: Repair gut integrity
Since SIBO always causes leaky gut, it is important to rebuild the integrity of the intestinal membranes. One of the best ways to do this is by using bone broth. Bone broth is high in glutamine and glycine, both of which are essential in healing the gut. They are emphasized in both the SCD and GAPS diets. Drink 1-4 cups of bone broth daily. You can also use it to make soups. Recipes for bone broth can be found online or in Nourishing Traditions.
If you can’t take the bone broth, you can use l-glutamine, which can also be used along with the bone broth. The best way to take it is to get the l-glutamine powder and take 1 teaspoon three times daily mixed with food. Other remedies that help heal the gut include chamomile tea (one cup three times daily), deglycyrrhizinated licorice (2 capsules three times daily), and colostrum powder, one teaspoon twice daily.
Additional Resources
For resources on the SCD diet, got to:
You can also consult any of the following books on the SCD diet.
- Healing Foods: Cooking for Celiacs, Colitis, Crohn's and IBS
by Sandra Ramacher
- Recipes for the Specific Carbohydrate Diet: The Grain-Free, Lactose-Free, Sugar-Free Solution to IBD, Celiac Disease, Autism, Cystic Fibrosis, and Other Health Conditions
by Raman Prasad
- Grain-Free Gourmet
by Jodi Bager & Jenny Lass
- Eat Well, Feel Well: More Than 150 Delicious Specific Carbohydrate Diet(TM)-Compliant Recipes
by Kendall Conrad
For resources on the GAPS diet go to:
- www.gaps.me (Dr. Natasha Campbell-McBride site)
- www.gapsguide.com (Baden’s site)
- www.gapsdiet.com
- www.gutandpsychologysyndrome.com (Intro Diet)
You can also consult any of the following books on the GAPS diet.
- Gut and Psychology Syndrome: Natural Treatment for Autism, Dyspraxia, A.D.D., Dyslexia, A.D.H.D., Depression, Schizophrenia
by by Dr. Natasha Campbell-McBride (great egg-free recipes)
- Gaps Guide
by Baden Lashkov
For information on the Paleo diet go to:
You can also consult any of the following books on the Paleo diet.
- Primal Body, Primal Mind: Beyond the Paleo Diet for Total Health and a Longer Life
by Nora Gedgaudas
- The Primal Blueprint: Reprogram your genes for effortless weight loss, vibrant health, and boundless energy (Primal Blueprint Series)
by Mark Sisson
- Practical Paleo: A Customized Approach to Health and a Whole-Foods Lifestyle
by Diane Sanfilippo
For personal consultations contact Thomas Easley (co-author of this article and an expert on SIBO) at 334-804-6830 or eclecticherbalist@gmail.com
Steven's Articles
-

-
Eucommia Bark
A superior tonic that promotes kidney, structural,…
January
-

-
Goldenthread, Phellodendron, and Yellow Root
Three herbal remedies containing the infection-fighting…
-

-
Teasel
A traditional herb for healing bones and joints…
-

-
Barberry and Healthy Personal Boundaries
A thorny shrub for fighting infections and supporting…
December
-

-
The Evidence for Berberine
A yellow alkaloid found in traditional infection-fighting…
-

-
The Sensible Use of Caffeinated Herbs
Kola nuts, guarana, and yerba mate and other herbs…
-

-
The Health Benefits and Problems with Coffee
This popular caffeinated beverage can be beneficial…
October
-

-
Understanding Caffeine & Cellular Adaptation
Preserving the power of caffeine's buzz and the…
September
-

-
Horseradish
A pungent spice for aiding protein metabolism…
-

-
Banaba or Crepe Myrtle
A beautiful tree from Southeast Asia whose leaves…
August
-

-
Monkeyflowers
Flower essences to help see ourselves more clearly…
-

-
Mariposa Lilies
Strengthening the bond between mother and child…
-

-
The Noble Bay Leaf
A common kitchen herb for aiding digestion and…
-

-
Epimedium: Horny Goat Weed
A circulatory stimulant and kidney yang tonic…
July
-

-
The Medicinal and Nutritional Benefits of Apricots
A nutritious fruit and valuable medicinal seed for coughs

